Articles
31 Posts found
Oral dydrogesterone treatment du...
By Medevista Official
consecutive pregnancy losses before 20 weeks of gestation (with the same partner) (2). Despite several well established etiologic factors, the cause of recurrent pregnancy loss (RPL) cannot be determined in almost 50% of cases. It was suggested that these unexplained RPLs might be due to immunologic factors (3). A successful pregnancy depends on tolerance of a semiallogenic embryo/fetus by the maternal immune system. It is believed that this tolerance depends on the interactions of various cytokines excreted by maternal and fetal cells at the site of implantation. A shift from proinflammatory T-helper (Th)1 cell-dependent cytokines to Th2-dependent anti-inflammatory cytokines seems to be a characteristic of a successful pregnancy .
Read More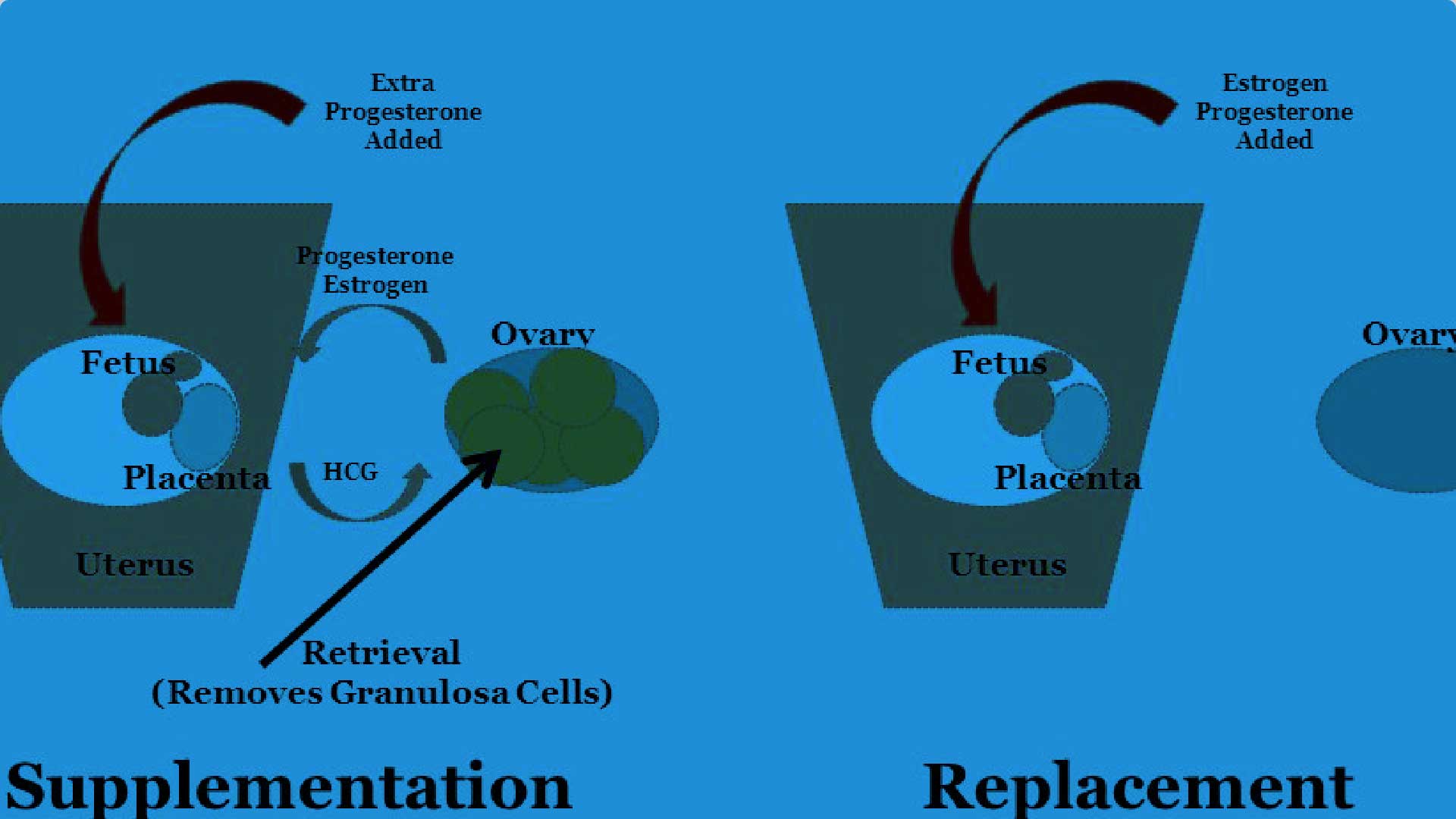
A Phase III randomized controlle...
By Medevista Official
Luteal phase support, in conjunction with gonadotropin-releasing hormone analogs, is routinely performed during in vitro fertilization (IVF) procedures to overcome luteal phase progesterone deficiency induced by ovarian stimulation (Practice Committee of the American Society for Reproductive Medicine, 2008; Palomba et al., 2015). Progesterone supplementation or human chorionic gonadotropin (hCG) are commonly administered, although hCG is associated with a higher risk of ovarian hyperstimulation syndrome than progesterone (van der Linden et al., 2015). A systematic review demonstrated that the use of progestogens in IVF was associated with an improvement in the live birth rate (van der Linden et al., 2015). Progesterone can be administered orally, vaginally, rectally, subcutaneously or intramuscularly, although the vaginal route is preferred in the majority of IVF centers globally (Vaisbuch et al., 2012). Indeed, oral administration of progesterone is associated with low bioavailability (due to a substantial firstpass metabolism) and side effects, such as somnolence (Shapiro et al., 2014), while daily intramuscular administration can lead to pain at the injection site, and local abscess (Ghanem and Al-Boghdady, 2012). In contrast, vaginal administration of progesterone can be associated with vaginal irritation, discharge and bleeding (Ghanem and Al-Boghdady, 2012). Therefore, there is an ongoing need for an effective, well tolerated and safe treatment that could also help improve patient satisfaction, convenience and compliance.
Read More
The Influence of Oral Dydrogeste...
By Medevista Official
Progesterone maintains pregnancy by enhancing uterine quiescence [1]. During early pregnancy, the syncytiotrophoblast secretes human chorionic gonadotropin (hCG), which stimulates progesterone production in the corpus luteum by preventing regression of this tissue [2]. After seven to nine weeks of gestation, progesterone is directly secreted by the syncytiotrophoblast [2, 3]. Low serum hCG or progesterone levels may predict first trimester abortions [4]. During early pregnancy in women with threatened abortion, progesterone levels were lower in those who had a subsequent miscarriage than in those whose pregnancies continued to fetal viability [5]. Moreover, progesterone receptor antagonists may induce abortion or labor by increasing myometrial contractility and excitability throughout pregnancy
Read More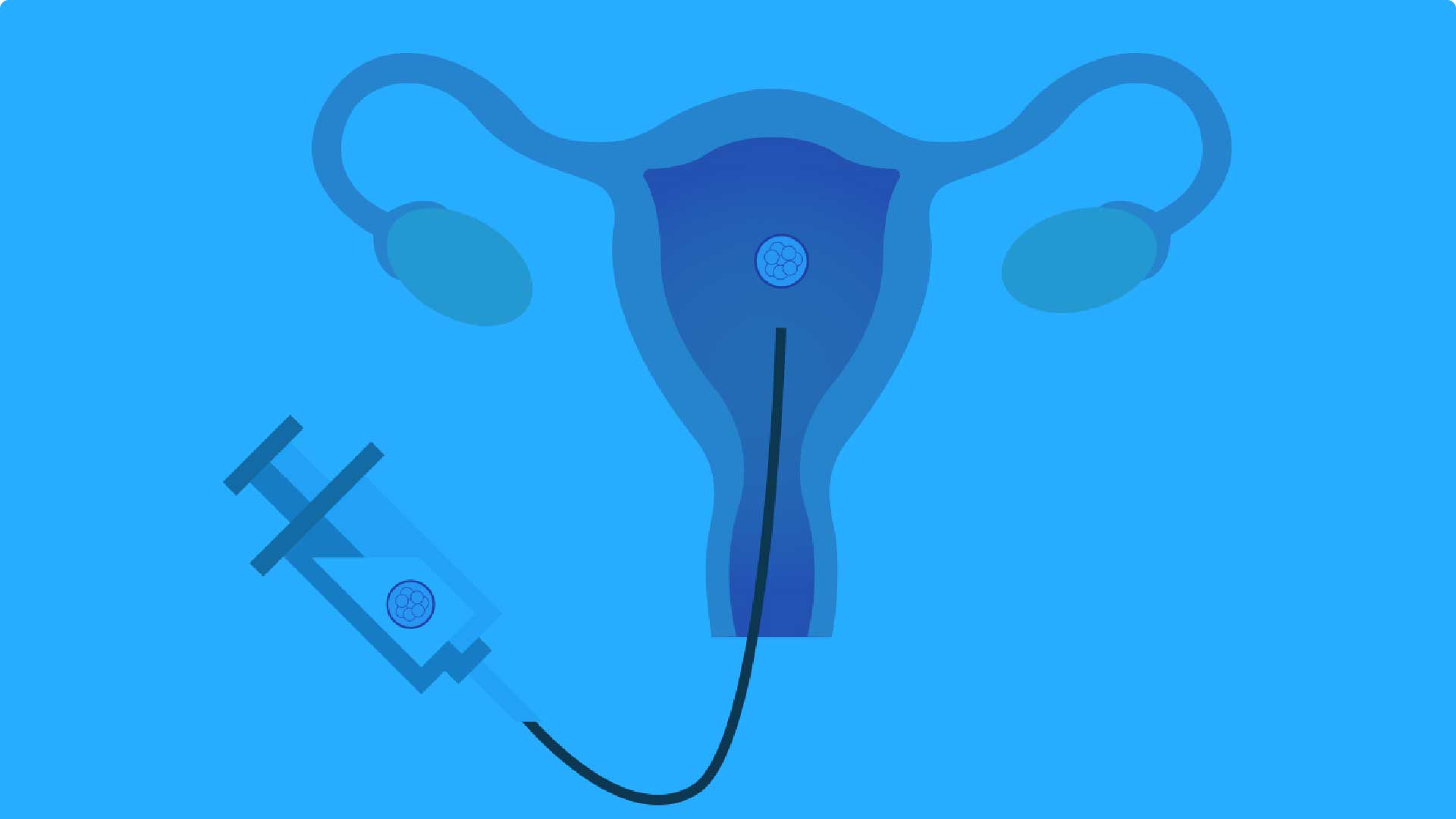
Oral dydrogesterone vs vaginal ...
By Medevista Official
Progesterone is needed to maintain early pregnancy, and progesterone supplementation in assisted reproduction technology (ART) cycles is a well-accepted procedure (Shapiro et al., 2014; Holmdahl et al., 1971; van der Linden et al., 2015). Luteal phase deficiency affects women undergoing ART for many reasons. The most widely accepted theory posits that luteal phase deficiency originates from premature negative feedback on LH secretion in the pituitary caused by supra-physiological levels of steroids during controlled ovarian stimulation (COS) sustained after oocyte aspiration by multiple corpora lutea (van der Linden et al., 2015; Fatemi 2009).
Read More
Oral dydrogesterone for luteal p...
By Medevista Official
Oral dydrogesterone has been used for luteal phase support on an empirical basis since the early days of in vitro fertilization (IVF) treatment. Systematic comparisons of oral dydrogesterone with vaginal progesterone, so far considered to be the standard of care, started to appear in the middle 2000s. Recently, a large, randomized, double-blind, double-dummy phase III trial on the use of daily 30 mg oral dydrogesterone versus daily 600 mg micronized vaginal progesterone for LPS in IVF was published. This company-sponsored trial confirmed the efficacy findings from previous independent researchers and firmly established the noninferiority of daily 30 mg oral dydrogesterone for luteal phase support. Despite oral administration and first pass through the liver, dydrogesterone was as well tolerated as vaginal progesterone in safety analyses. Moreover, no new fetal safety concerns have arisen from that trial. Given the widespread preference of women for an oral compound, dydrogesterone may well become the new standard for luteal phase support in fresh embryo transfer IVF cycles.
Read More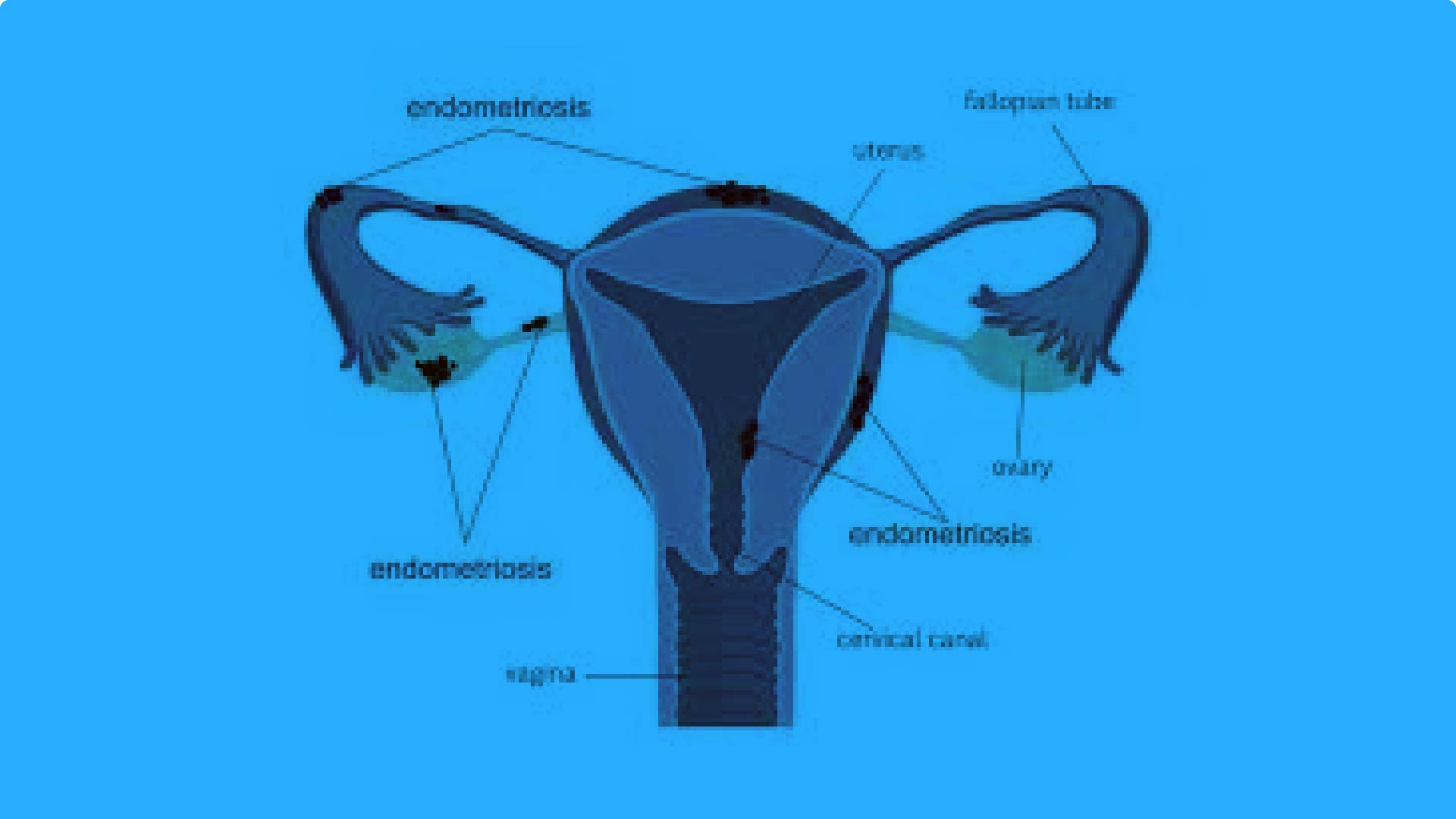
Long term treatment of endometri...
By Medevista Official
Endometriosis is a chronic, recurrent disease associated with debilitating pain and severely reduced quality of life in many afected women [1–3]. In the absence of a defnitive cure, the main management options in endometriosis comprise surgery, hormone therapy, or a combination of these two approaches. Excision of endometrial lesions by laparotomy provides a rapid alleviation of symptoms, but lesion recurrence rates are high, estimated at 40–50% at 5 years [4]. For these women, hormone therapy postoperatively can reduce lesion recurrence and extend the pain-free period [5, 6]. Hormone therapy is also widely used as a frst-line empirical therapy in symptomatic women and in those cases where surgery is considered impossible or is rejected by the patient.
Read More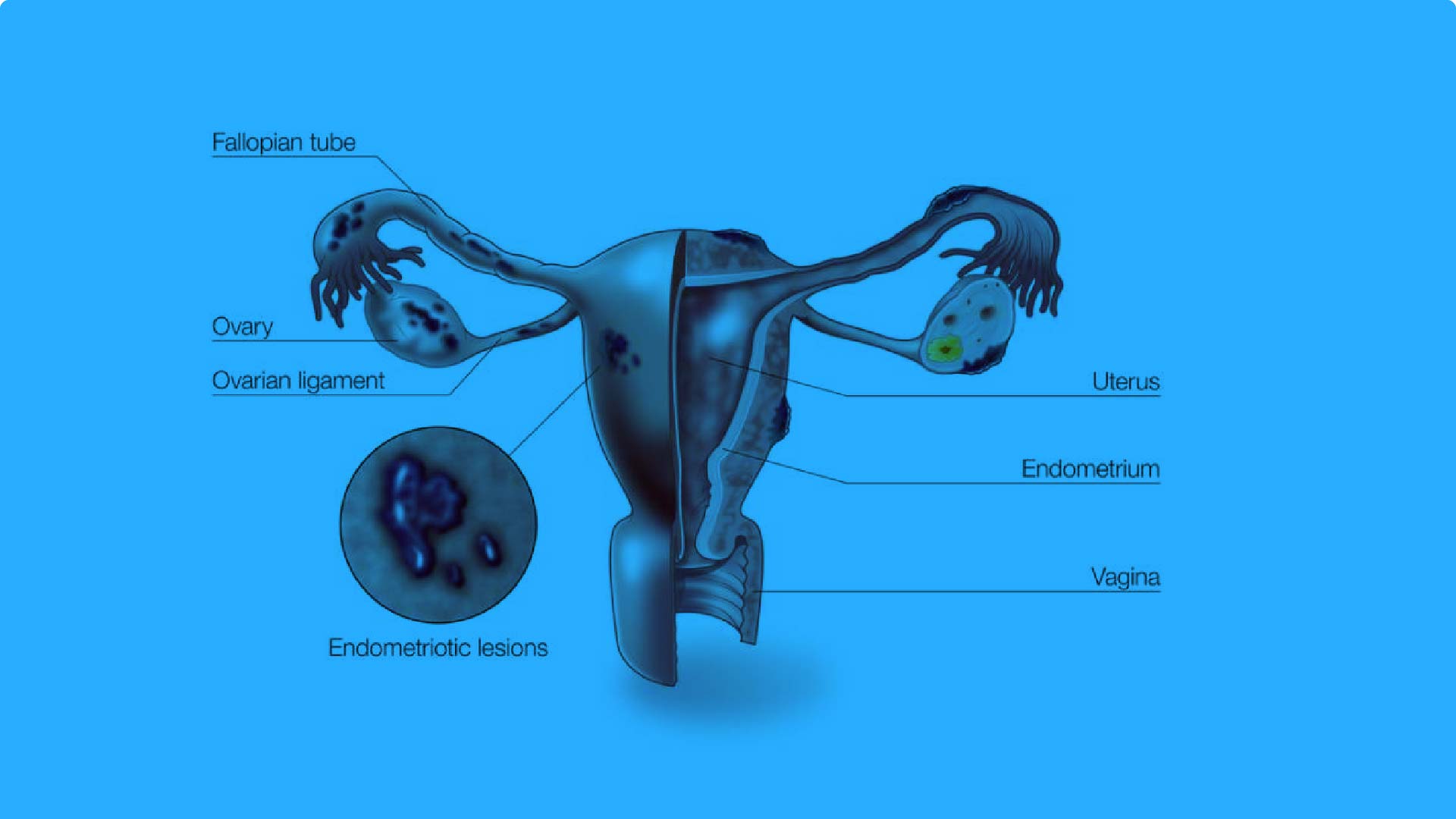
Dienogest 2 mg Daily in the Trea...
By Medevista Official
Relative to adults, there are limited data on the frequency and symptoms of endometriosis in adolescents,1,2 although many women first report symptoms in their teens or earlier.3e5 Approximately 5% of girls aged 15-19 years report severe dysmenorrhea not alleviated by combined oral contraceptives (COCs) and pain medication, a condition suggestive of endometriosis.6,7 Endometriosis has been diagnosed using laparoscopy in young adolescents and young women (younger than 19-21 years) with dysmenorrhea and chronic pelvic pain at rates between 35% and 70%.2,8e10 The most common treatments for adults with endometriosis are medications to reduce pain (for example, nonsteroidal anti-inflammatory drugs [NSAIDs]), hormonal therapies, and laparoscopic surgery.11 The rationale for hormonal therapies is to reduce circulating concentrations of estrogen, which decreases endometriotic lesion size and symptoms. Hormonal therapies available include COCs (unapproved by regulatory authorities for use in endometriosis), progestins, gonadotropin-releasing hormone Andreas D. Ebert has received consulting fees and reimbursement from BayerGermany, Jenapharm Germany, Takeda Germany, and Gedeon Richter. Liying Dong, Martin Merz, Bodo Kirsch, Maja Francuski, Kerstin Gude, and Christian Seitz are fulltime employees of Bayer AG. Horace Roman has received consulting fees from Nordic Pharma, Bayer, Covidien, Ipsen, and Plasma Surgical Ltd. Pia Suvitie has received consulting fees and reimbursements from Gedeon Richter Nordics, MSD,Covidien, and Olympus. Olga Hlavackova and Bettina Bottcher indicate no con € flicts of interest.
Read More
Evaluation of the efficacy, safe...
By Medevista Official
Dysmenorrhea is a pathological symptom of menstruation. During dysmenorrhea, the pain occurs primarily in the lower abdomen and back (1, 2), and has a considerable impact on the quality of life (QOL) and work of affected women (1). Dysmenorrhea is divided into the categories of primary dysmenorrhea and secondary dysmenorrhea. Dysmenorrhea without underlying organic disease is diagnosed as primary dysmenorrhea (3). It involves increased production of endogenous bioactive substances such as prostaglandin in the late secretory endometria during the menstrual cycle, and it results in uterine hypercontraction, with vasospasm and ischemia in the myometrium at the time of menstruation (4). Therefore, effective Received May 22, 2019; revised September 9, 2019; accepted September 12, 2019; published online November 11, 2019. Y.O. is a medical expert contracted to Mochida Pharmaceutical Co., Ltd. and reports consulting fees from Mochida during the conduct of the study. K.H. was an employee of Mochida Pharmaceutical Co., Ltd., during the conduct of the study. S.K. was an employee of Mochida Pharmaceutical Co., Ltd., during the conduct of the study. Sponsored by Mochida Pharmaceutical Co., Ltd.
Read More
Dienogest and deep infiltrating ...
By Medevista Official
Endometriosis is an estrogen-dependent inflammatory disease defined as the presence of endometrial-like tissue outside the uterus. In its severe form, deep infiltrating endometriosis (DIE), which is marked by endometrial implants below the peritoneum, can affect the rectosigmoid colon, rectovaginal septum, uterosacral ligament, bladder, and ureters.
Read More