Articles
31 Posts found
Effect of estradiol valerate on ...
By Medevista Official
Letrozole is as effective as clomiphene citrate for induction of ovulation in patients with PCOS. Adequate endometrial development is required for pregnancy to occur, and pregnancy rates were found to be higher when the endometrium reached at least 10 mm thickness.
Read More
The use of estradiol for luteal ...
By Medevista Official
The role of E2 in the follicular phase of the menstrual cycle is well documented. E2 is essential for endometrial priming, but it is also responsible for proliferation of uterine surface epithelium, glands, stroma, and blood vessels. The role of E2 in the luteal phase, including the preparation of the endometrium forembryo implantation, remains unclear, and its depletion in the human luteal phase does not appear to adversely affect the morphological developmental capacity of the endometrium
Read More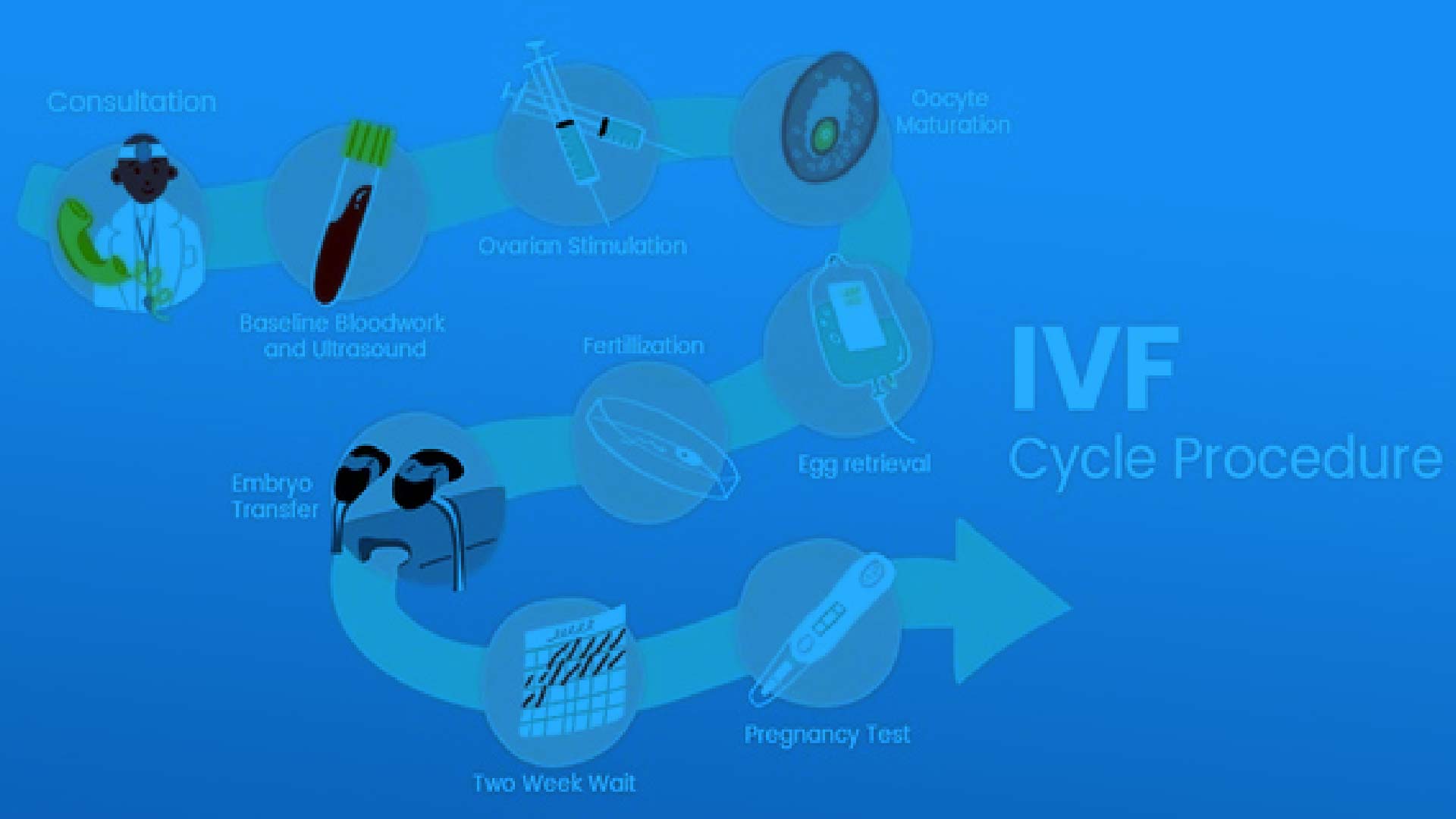
Endometrial preparation for in v...
By Medevista Official
In vitro fertilization (IVF) and embryo transfer are an established and successful form of treatment for infertility, with continuously improving cumulative pregnancy rates reaching 57.8% before age of 40, after 3 cycles of IVF (1). However, high success rates with IVF are achieved at the risk of 2 major complications, namely, multiple pregnancy and ovarian hyperstimulation syndrome (OHSS). All assisted conception techniques are associated with an increase in the rate of multiple pregnancies because several embryos must be transferred to achieve high pregnancy rates. Moreover, to have several embryos available for transfer, ovarian stimulation is required, which places the patient at risk for the development of OHSS. Although there are many strategies to prevent and predict OHSS, none is universally successful. The only way to prevent OHSS reliably would be to avoid stimulating the ovaries. Because stimulated ovaries are not necessary for treatment by in vitro maturation (IVM) of immature oocytes, this technique has received increased attention in recent years.
Read More
Clinical Experience With Oral Mi...
By Medevista Official
The success rates of in-vitro ferlizaon (IVF) have plateaued over the last few years. Various factors affect the outcomes, endometrial recepvity being one such. In IVF with own oocytes, endometrial growth is brought about by the estrogen secreted by the mulple follicles recruited as a result of controlled ovarian hypersmulaon. In donor egg IVF however, endometrium has to be prepared arficially with hormone replacement. Various regimens have been suggested for the same but a consensus regarding the opmal method is sll lacking. This small observaonal study takes a look at the efficacy of oral micronized estradiol valerate in improving endometrial thickness in women undergoing donor-egg IVF both with fresh and frozen-thawed embryos.
Read More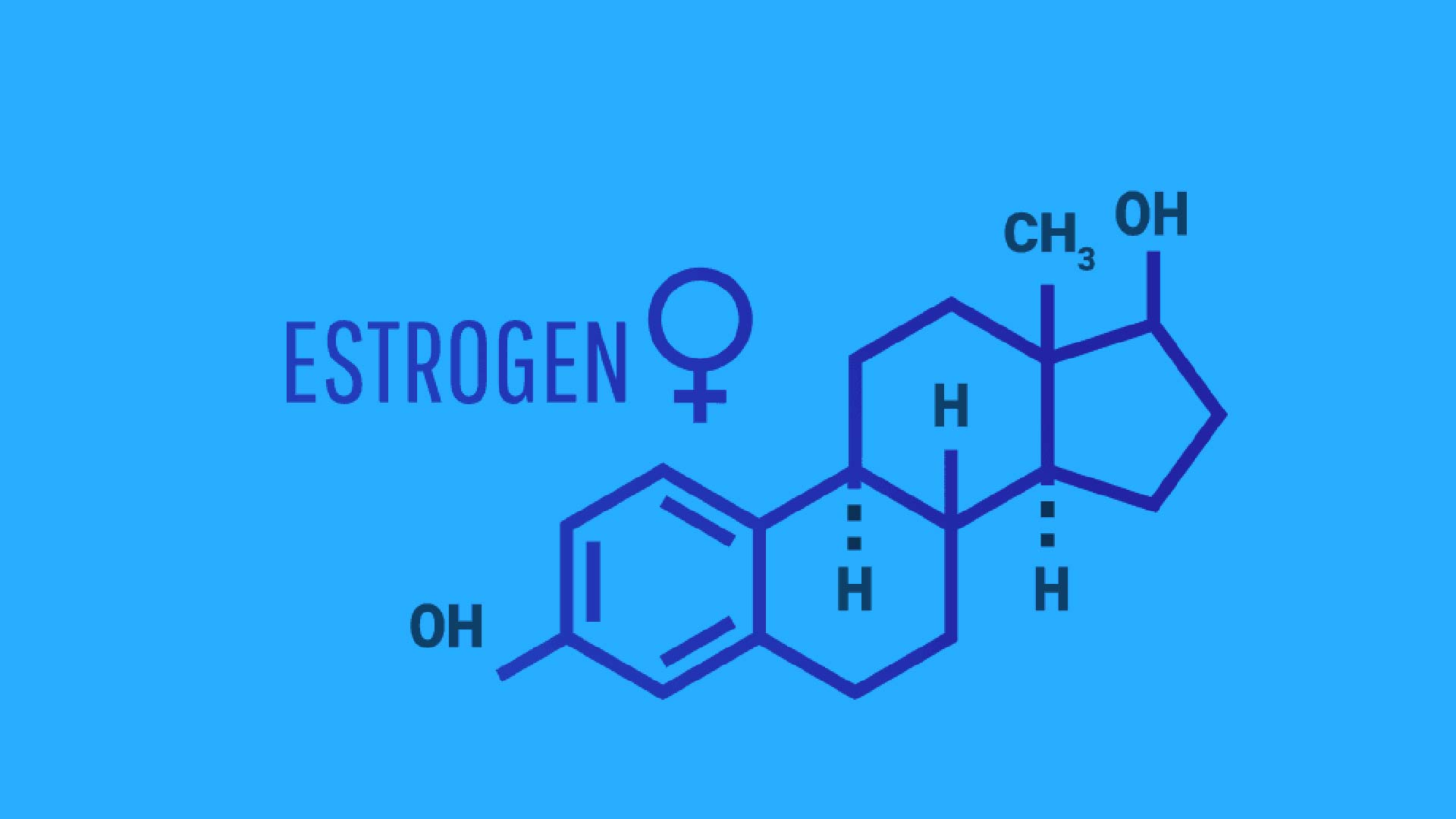
Effect of estrogen priming throu...
By Medevista Official
Purpose To verify whether a novel protocol administering E2 during the luteal phase of the preceding cycle and during ovarian stimulation in GnRH antagonist cycle could enhance follicular response and hence improve outcomes in poor responders. Methods In this retrospective analysis, a total of 155 poor responder patients subjected to IVF/ICSI were analyzed. All the patients had history of more than one prior IVF cycle failure with poor response (less than 5 oocytes retrieved and/ or maximal E2 level less than 500 pg/mL) by using conventional long agonist or antagonist protocol. In luteal E2 treatment protocol (n086), oral estradiol valerate 4 mg/day was initiated on luteal day 21 and either stopped at menstrual cycle day 3 (Protocol A, n028) or continued during the period of ovarian stimulation until the day of hCG injection (Protocol B, n058). IVF parameters and pregnancy outcome of luteal E2 treatments group were compared with a standard GnRH antagonist protocol (n069) which the patients received no hormonal pretreatment. Results Compared to standard GnRH antagonist protocol, cancellation rate was lower with luteal E2 group (15.1% vs 37.7%, p<0.01). Moreover, patients treated with luteal estrogen resulted in an increased number of oocytes retrieved (4.5±2.9 vs 3.2±1.9; p<0.01). A trend toward increase in number of normally fertilized embryos (2.9±2.1vs 2.3±1.9; p00.043), and increased prevalence of good quality embryos (51.2% vs 25%; p00.047) were noted. Comparing protocol A and B, there were no significant difference between embryologic data, however there were slight increase in ongoing pregnancy rate in protocol B compared to A (27.1% vs 20%, p00.357), although statistical significance was not achieved. Conclusion Estrogen priming through luteal phase and stimulation phase improved ovarian responsiveness and this may lead to an increase in pregnancy rate in poor responders with failed cycle.
Read More
A Comparison of Prevention and T...
By Medevista Official
Most recent publications offer the opportunity not only to look at large studies, but also to be able to compare the effect of the use of micronized progesterone or dydrogesterone for prevention of recurrent (habitual) miscarriage. Micronized progesterone and dydrogesterone have a similar partial effect pattern, which does not induce unwanted effects, when used in pregnancy. Also their major actions regarding implantation, preparation of the endometrium, blood flow increase, spiral artery development, uterine quiescence, cervical rigidity and protection of the semi-allogenic fetus not to be attacked by the maternal immune system, for instance regulating the Th1- and Th2-cytokines to establish and continue to have a dominance of Th2-cytokine action and protection against these effects which are associated with lower circulating progesterone. Both studies under consideration have included women with a history of three or more previous miscarriages and other non-endocrine or endocrine abnormalities have been ruled out.
Read More
Assessment of sub endometrial bl...
By Medevista Official
Recurrent spontaneous miscarriage is defined as three or more consecutive pregnancy losses within 20 weeks of gestation. The etiology of this disorder remains unsolved in nearly 50% of these cases.1 An unsupportive endometrium, leading to abnormal implantation, is considered to be a key factor contributing to idiopathic recurrent spontaneous miscarriage (IRSM). Structural and functional modifications of the endometrial vasculature are essential for endometrial receptivity during the implantation window.2–4 Uterine perfusion is one of the major factors regulating uterine receptivity and is of great importance in achieving a normal pregnancy.5 Increased uterine artery vascular resistance and reduced uterine blood flow have been used as predictors of high-risk pregnancies, which also may be the likely causes of IRSM.
Read More
A systematic review of dydrogest...
By Medevista Official
Threatened miscarriage is defined by the National Library of Medicine, Medical Subject Headings (2012 MeSH), as bleeding during the first 20 weeks of pregnancy while the cervix is closed. It is the most common complication in pregnancy, occurring in 20% of all pregnancies. The condition may progress to miscarriage in approximately one-half of cases [1,2], or may resolve. There are problems of definition, as the bleeding may include anything from spots of blood to potentially fatal shock. The treating physician is faced with the question whether any treatment can effectively prevent the pregnancy from being miscarried. Progestational agents have been prescribed since the 1950s in order to prevent miscarriages. There are many theoretical data to support the use of progestagens. Progestagens enhances implantation, affect the cytokine balance, inhibit natural killer cell activity at the feto-maternal interface, inhibit the release of arachidonic acid, prevent myometrial contractility and prevent cervical dilatation. Activation of progesterone receptors on lymphocytes results in the synthesis of a protein known as progesterone-induced blocking factor (PIBF) [3]. PIBF favours the production of asymmetric, pregnancy-protecting antibodies.
Read More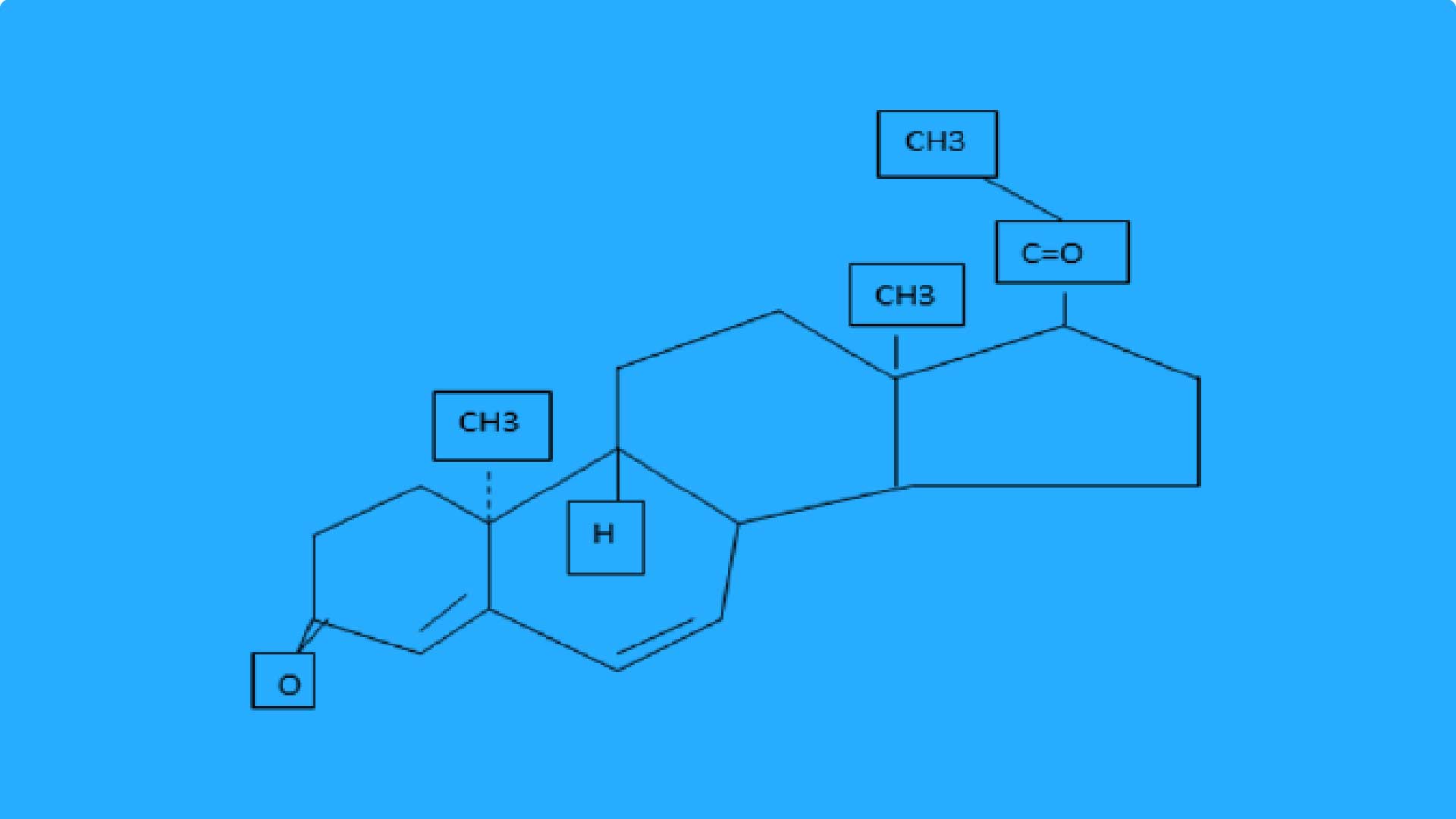
Comparison of oral dydrogesteron...
By Medevista Official
It is well established that luteal function is compromised in in vitro fertilization (IVF) cycles and studies on cases undergoing IVF demonstrated that there was a significant reduction in pregnancy rates without lutealphase support (LPS) (1-3). In the absence of luteal-phase support, the area under the curve for progesterone is suboptimal and accompany by premature luteolysis, short luteal phase and early bleeding (4, 5). Progesterone is necessary for implantation and for the early development of the fertilized ovum. In response to progesterone, the glands become tortuous and secretory and there is an increase in stromal vascularity, thus making the endometrium both morphologically and functionally well prepared for implantation
Read More